
Weight loss is so much more than eat less move more. Research has shown that only ≈20% of overweight individuals are successful at long-term weight loss. (weight loss being defined as losing at least 10% of initial body weight and maintaining the loss for at least one year [17]).
So what affects an individuals weight loss success?
This blog looks at a recent study which states that “the internal factors resulting from the complex pathophysiology of obesity such as hormonal imbalance, nutritional and metabolic factors can counter a persons efforts to lose weight [18]. “
Additional factors that play a crucial role in upregulating or downregulating metabolism and weight loss include:
- previous weight loss attempts
- sleep habits
- meal timings
- medications
- menopause
- insulin resistance
OBESITY STATS
The World Health Organization (WHO) describes overweight and obesity as an abnormal condition that impairs health causing 4 million deaths annually [1].
Across the globe, the prevalence of overweight and obesity between 1980 and 2013 increased by 27.5% among adults [2].
Since 1980, a third of the global population has been determined to be obese or overweight [3].
The exact reasons for obesity remain unknown, but there is a complex link between biological, psychosocial and behavioural factors [4].
Further, genetic disposition to obesity [5], unhealthy diet including highly processed foods [9], sedentary lifestyle, disturbed circadian rhythm [6, 7], underlying medical conditions and certain medications [8] all add to the global obesity pandemic [10, 11].
Complexity arises in identifying the real reasons for not losing weight because most of these factors are interlinked, forming reinforcing loops leading to the struggles people have with trying to lose weight.
Although many individuals attempt to lose weight, not everyone achieves optimal success.
Studies point out that weight loss eventually slows down, stagnates or reverses in 85% of the cases
CURRENT OBESITY TREATMENT
Current obesity treatment strategies include diet, exercise, bariatric surgery, and a limited but growing repertoire of medications. Individual weight loss in response to each of these strategies is highly variable.
This blog reviews a recent study published in March 2024 which looked at factors that may potentially contribute to an individuals variable response to weight loss.
Well-recognized factors associated with weight loss capacity include diet adherence, physical activity, sex, age, and specific medications.
However, differences in weight loss persists in response to behavioural, pharmacological and surgical interventions.
Plus the body soon adapts to an energy (calorie) deficit.
Adaptation to energy deficit involves complex feedback mechanisms, and inter-individual differences likely arise from genetic factors, as well as differential responses in neurohormonal mechanisms (including gastrointestinal peptides), metabolic efficiency and capacity of tissues, non-exercise activity thermogenesis, thermogenic response to food, and in gut microbiome.
THERE IS NO ONE SIZE FITS ALL
The aim of this study was to gain a better understanding of the factors involved an individuals variability in response to therapies with a view to moving towards a more personalized approach to weight loss and the treatment of obesity.
What could be the reasons for not losing weight even after following a weight loss program?
Studies recommend that a modest weight loss of 5 to 10% significantly improves parameters such as blood glucose levels, blood pressure, inflammatory markers and lipid profiles. [12,13,14].
Hence, to mitigate the risk of developing related metabolic ailments or alleviate existing chronic conditions, individuals with obesity are often advised to reduce weight by creating an energy deficit (eat less /move more) [15].
However simple this advice might seem; it doesn’t seem to work for many [16]. I’m sure many of you reading this can relate.
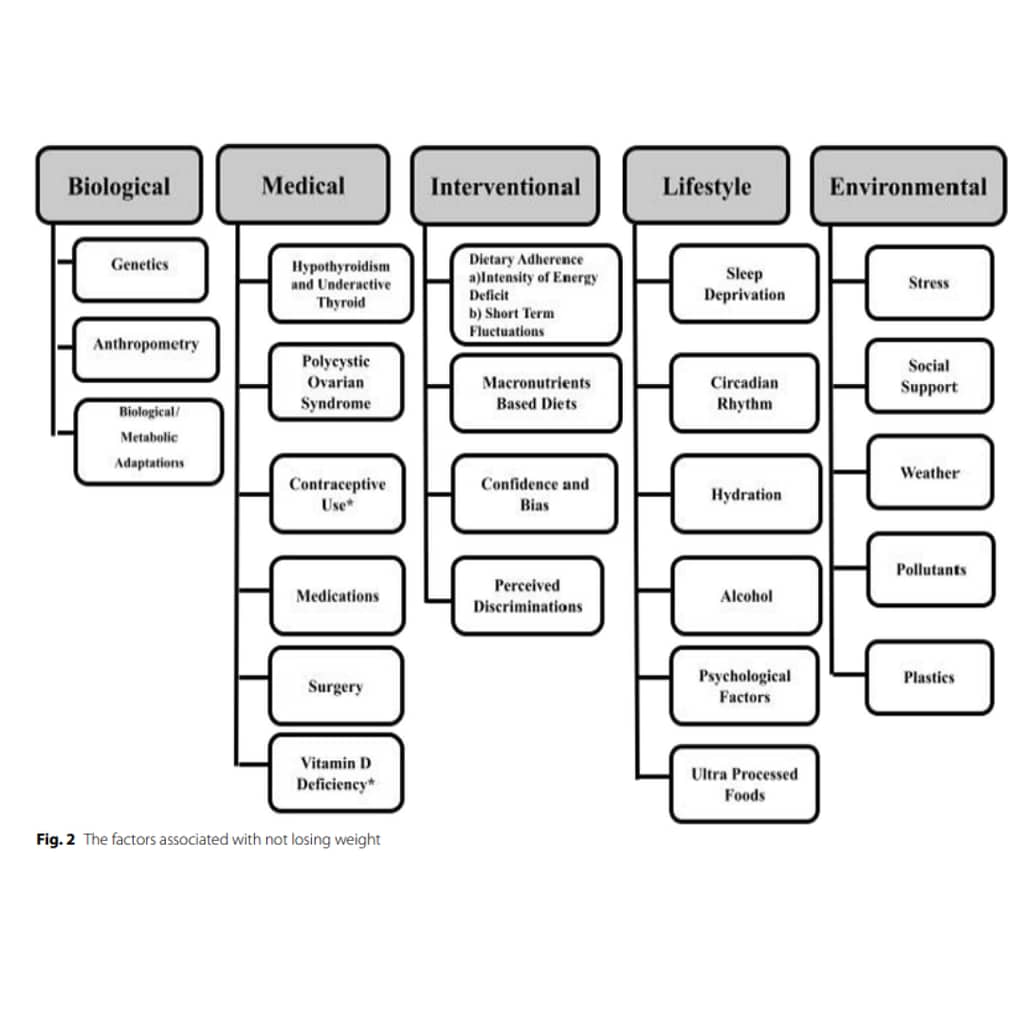
The study reviewed in this blog looked at 5 specific areas that may affect individual variability when it comes to weight loss:
- (1) Biological
- (2) Medical
- (3) Interventional
- (4) Lifestyle
- (5) Environmental
Biological factors affecting Weight Loss
Biological factors looked at that may hinder weight loss include:
- Genetics
- Anthropometry
- Metabolic adaptations
1. Genetics
The genetic component significantly contributes to obesity development, estimated with a heritability of 40–70%
The role of genetics in response to energy restriction is complex,
Genetic factors contribute to varied weight loss responses, other variables like age, sex, race, deficit accumulation and baseline weight make weight loss more challenging for specific individuals.
2. Anthropometry (the study of measurements/proportions of the human body)
In anthropology, factors like height, weight, body composition, size and BMI are considered.
Body size, influenced by fat-free mass, plays a vital role in weight loss outcomes. Further, initial success is crucial for eventual success in weight loss efforts.
Taller or heavier individuals with more fat-free mass typically have a higher basal metabolic rate, potentially facilitating quicker weight loss with similar calorie intake [29,30,31].
Conversely, shorter and lighter individuals may find weight loss more challenging.
Several studies have identified that those with a BMI > 30 kg/m2 struggle with recommended physical activity, whereas those with a BMI of 25 kg/m2 perform better [32,33,34,35,36,37].
Concluding for these trials, high adiposity (bodyfat) linked to low physical activity affects weight loss outcomes.
Weight loss success depends on follow-up frequency, initial BMI and initial weight loss.
Fewer follow-ups, lower initial BMI and minimal initial weight loss failed to maintain the lost weight beyond a year.

3. Biological /Metabolic Adaptations
In response to an energy deficit, (consuming fewer calories), the resting metabolic rate can drop notably (within days), disproportionately to body mass reduction.
This is known as metabolic adaptation – the body’s survival mechanism after significant weight loss.
A study on perimenopausal women linked larger metabolic adaptation to a prolonged time in achieving weight loss goals, suggesting strategies to decrease a larger metabolic adaptation/energy deficit, may expedite weight loss.
Metabolic adaptation partly explains slower weight loss in later stages of energy deficit. Many women will be able to relate to losing weight quicker at the start of a weight loss program with results then stagnating.
This is because the body has a strong homeostatic drive to maintain a higher weight and to gain lost weight – as the body recognises this as ‘safe’.
The problem with yo-yo dieting
After significant weight loss, highly insulin-sensitive and fuel-exhausted fat cells will secrete low leptin (the hunger hormone that tells us when we are full), hypothesized to be more pronounced in individuals intermittently maintaining, losing and gaining weight, aka yo-yo dieters.
Changes in neuronal activity in the brain in response to a prolonged energy deficit can trigger appetite, reduce satiety and promote positive energy (calorie) balance.
Additional mechanisms, like changes in gut signals and enhanced metabolic regulation, can also foster positive energy balance during or after weight loss.
In conclusion, individuals with a previous history of weight loss attempts may carry forward the metabolic debt, making it difficult to lose weight with a mild calorie deficit from their calculated daily energy expenditure.
Medical issues affecting Weight Loss
There are many medical reasons for not losing weight. For the purpose of this study large-effect factors were reviewed including:
- Hypothyroidism & underactive thyroid
- Polycystic ovarian syndrome
- Contraceptive use
- Medications
- Surgery
- Vitamin D deficiency
4. Hypothyroidism and Underactive Thyroid
The thyroid influences metabolism.
Thyroid hormone deficiency is known as Hypothyroidism.
Whilst, due to a lack of evidence), there isn’t a clear consensus that hypothyroidism directly causes obesity, experiments show treatment effects weight loss (and related markers).
A study revealed a 17% reduction in resting energy expenditure with a serum TSH increase (0.1–10 mU/L) from levothyroxine medication, hindering weight loss attempts and promoting weight gain.
Another study reported hypothyroid patients lost 2.25 ± 2.01 kg of body weight within 12 months after achieving normal thyroid levels through medical treatment. Although small, combining this effect with lifestyle measures may enhance outcomes.
In conclusion, a normal functioning thyroid is crucial during weight loss interventions to counteract hypothyroidism’s hindrance to weight loss efforts.
Consuming iodine rich foods and iodine supplements may help support the thyroid.
Thyroid levels can be checked via a blood test.
5. Polycystic ovarian syndrome
Weight gain and obesity can contribute to PCOS/PCOD development in genetically predisposed women.
In particular psychological factors, including depression and low self-control, may hinder weight loss efforts in some PCOS patients.
However, a systematic review of 14 lifestyle intervention studies found no statistically significant difference in weight loss between women with and without PCOS.
Another study comparing a very low-calorie diet for 12 weeks showed no significant difference in weight loss between women with and without PCOS.
In conclusion, psychological effects seem more impactful than physiological changes, further studies are required.
6. Contraception use
Recent evidence suggests no clinically and statistically significant short or long-term effects of oral contraceptives on weight in women with normal or higher BMI.
However, a recent secondary analysis suggested an association between oral contraceptive use and weight gain after weight loss, although, only a small number of individuals were studied for any conclusive evidence.
The available evidence is also insufficient to estimate the effect of oral contraception on weight loss outcomes during energy (calorie) restriction.
As the jury is out, this warrants future clinical trials for a better understanding of how contraception may or may not affect weight loss success.
7. Medications
Insulin therapy affects weight loss in diabetic individuals, triggering appetite, causing hypoglycemia and increasing body fat.
Beta-blockers have reported long-term weight gain, but their effect on weight loss in response to hypocaloric regimens is unclear.
Antidepressants have indicated an association with obesity in observational studies and there is some evidence suggesting their role in weight gain but causal links and their effect on weight loss outcomes during energy restriction require more investigation.
Similar to antidepressants, antibiotics impact also requires future study with large sample size studies.
8. Surgeries
Bariatric surgeries and other major surgeries restricting movement, such as knee replacement surgeries, may also affect weight loss success.
The loss of weight after bariatric surgery might be due to the effect on hormones.
(The removal of the foregut may lead to a hormonal upregulation of pancreatic peptide YY, glucagon-like peptide-1 (GLP-1) and gastric inhibitory polypeptide hormones).
These factors will improve satiety and reduce hunger, as well as downregulate hunger hormone ghrelin with a subsequent decrease in food intake.
As time proceeds, however, there will be changes in the levels of the hunger hormones ghrelin and leptin resulting in weight regain as well as insufficient weight loss.
Additionally, after surgery in most cases, physical inactivity and water retention can lead to weight loss failures.
Elderly patients will not lose as much weight as younger patients due to aging.
Also, behavioural and lifestyle changes are found to be crucial for long-term success even after bariatric surgery.
Studies on other surgeries, like knee replacement surgeries that limit movement, were found to track weight gain and further investigation on the impact of common surgeries on energy status is necessary.

9. Vitamin D Deficiency
Studies indicate a negative correlation between higher BMI/body fat and lower vitamin D concentration.
A placebo trial of overweight or obese women with vitamin D deficiency showed no significant difference in weight loss between those receiving oral vitamin D3 and the placebo. These effects were also consistent with a previous similar trial.
However, the negative correlation does not necessarily mean causation: Vitamin D deficiency does not appear to obstruct meaningful weight loss during lifestyle intervention.
Interventional Factors
In this section, interventional factors affecting weight loss results reviewed include:
- Adherence (having significant impact)
- Macronutrient-based Diets
- Confidence and Bias
- Perceived Discrimination
- (The impact of physical activities were not in the scope of this study)
10. Dietary Adherence
‘Adherence’ being an individual’s ability to stick to dietary or exercise recommendations.
A year-long study on four popular diets on weight loss found a significant association (r = 0.60; p < 0.001) between self-reported adherence and weight loss, but the same was not true for diet type and weight loss (r = 0.07; p = 0.40) [81].
Similar observations occurred in another study assessing weight loss and dietary adherence across 3 popular diets. Regardless of the type of diet followed, one-year weight loss was greatest in the individuals who were most adherent.
Plus, previous dietary adherence levels are good predictors of future long-term weight regain.
In a study on premenopausal women, subjects who showed higher adherence during past low-calorie diet intervention regained 49.9 ± 8.8% of lost weight in two years follow-up, while the lower adherence tertile showed 96.8 ± 12.8% gain.
However, adhering to any lifestyle intervention poses a significant challenge.
For example, participants in a study showed higher adherence to a low-calorie diet but still regained half of their weight after 2 years.
A further study reported overall low adherence across all four intervention diets, with adherence declining over time.
A meta-analysis of 27 studies reported only a 60.5% adherence rate.
Adherence to intervention is positively associated with greater weight loss and a reduction of obesity risk factors.
Conversely, adherence it is negatively associated with factors like lack of knowledge, insufficient education about diet, inability to afford healthy food, limited awareness of the benefits of dietary recommendations, stress, unrealistic weight loss expectations, poor self-confidence and reduced motivation.
Initial weight loss success increases motivation and confidence, improves adherence and reduces chances of weight loss failure.
On the other hand, fluctuating results give mixed signals on the success of strategies and can disrupt adherence.
11. Adherence – Intensity of Energy Deficit
Initial weight loss directly correlates with the intensity of the energy deficit.
While there’s no specific definition for ‘low energy/calorie diets,’ intense interventions are around ~ 800 kcal per day, whereas a sustained deficit is 500–750 kcal less each day.
Whilst there is no agreement as to which is the most appropriate energy deficit intensity for weight loss, both an intense deficit intervention and a sustained deficit have a positive correlation between initial weight loss and adherence to the intervention.
The 500–750 kcal deficit model is relatively easier to follow and may enhance adherence.
Setting the right intensity involves individual motivation and preference, as a mismatch can lead to loss of motivation, and non-adherence, and hinder weight loss efforts.
12. Adherence – Short Term Fluctuations
Variations in glycogen levels (stored sugar in the muscles and liver), constipation and errors in weight or fat loss measuring techniques can cause short-term fluctuations or mistakes in recording progress.
A lack of improvements may demotivate individuals and affect adherence.
The study found that educating individuals about these is important to increase awareness and avoid derailing weight loss progress.
13. Macronutrient-based diets
Macronutrient compositions have been well studied and in particular, changing protein and carbohydrate compositions have been shown to have a significant effect on weight loss.
High Protein Diets
There is evidence that high-protein diets are beneficial for weight loss.
A meta-analysis showed that high-protein diets were modestly beneficial for weight loss compared to standard protein diets (~ 0.8 g/kg) .
Here’s 3 reasons how protein benefits weight loss success:
- In the longer term high-protein diets also tend to prevent muscle loss, which in turn can positively affect total energy expenditure (metabolism).
2. Protein also usually has a higher thermic effect which may partly contribute to additional energy expenditure. Of all the macronutrients, protein uses the most calories during the digestion process itself)
In contrast, a diet significantly lower in protein can affect energy expenditure negatively in the short and the longer term.
3. Protein also induces higher satiety as well.
Low Carbohydrate Diets
Ketogenic or lower carbohydrate diets (where the majority of the carbohydrate intake is substituted with fat intake) tend to show greater weight loss in a shorter (approx 24 weeks) duration.
Reasons for this weight loss include: Initial glycogen depletion, higher satiety, appetite suppression and greater metabolic efficiency.
However, if matched for calories, lower carbohydrate diets do not seem to be superior for fat loss compared to higher carbohydrate diets.
Hence, concerning carbohydrates, in the long-term, the amount in the diet is not significant regarding hindrance in weight loss.
Low Protein Diets
On the other hand, those on low protein diets may suffer from lean mass loss which will affect the resting metabolic rate in the long-term weight loss interventions.
Lean muscle mass maintenance also depends on regularly engaging in resistance (strength) training.
It conclusion it can be argued that as long as a diet meets a calorie deficit requirement and is sufficiently satiating along with supporting lifestyle interventions such as suitable activity to prevent lean mass loss, the variation in the macronutrient composition of the diet may not play a significant role as the reason for someone not being able to lose weight.
14. Confidence & Bias
The personal beliefs of a coach or practitioner about nutrition or exercise intervention may affect the response to behavioural or dietary intervention, and hence, it can directly affect adherence levels in subjects. This in turn can influence the weight loss experienced.
15. Perceived Discrimination
Individuals who feel judged by primary care providers for their obesity achieve less weight loss compared to those who do not perceive judgment.
Individuals who experienced more obesity stigma reported having less health utility.
Lifestyle Factors
Lifestyle factors evaluated that may hinder weight loss include:
- Sleep Deprivation
- Circadian Misalignment
- Hydration
- Alcohol
- Psychological Factors
- Consumption of Ultra Processed Foods
16. Sleep Deprivation
A 2 week study of moderate energy restriction found that the group sleeping for 8.5 h lost more fat compared to the 5.5-h sleep group (1.4 vs. 0.6 kg, p = 0.043).
The sleep-deprived group also lost more muscle mass, highlighting the importance of sufficient sleep during a weight loss journey.
Sleep-deprived individuals show hormonal changes promoting a protective effect on body fat with greater reductions in resting metabolic rate and increased hunger, possibly due to elevated ghrelin levels (hunger hormone).
Poor sleep quality is also linked to reduced muscle mass and, with even a small reduction in sleep (1.5 h over three weeks), reduced insulin sensitivity and increased weight gain.
Overall, the hormonal changes induced by sleep deprivation can make sustaining a restricted-energy diet challenging, leading to increased hunger levels and potentially hindering weight loss efforts.

17. Circadian misalignment—sleep and meals
Circadian rhythms influence various physiological processes through changes in environmental stimuli such as light and meals that can alter set rhythms of rest and wakefulness.
Daily patterns such as shift work creates circadian misalignment, impacting cortisol and melatonin levels. This can also reduce total daily energy expenditure, and decrease glucose tolerance and leptin levels, making weight loss challenging.
Moreover, delaying the main meal deterred the pace and the total amount of weight lost.
A study of women eating more calories at breakfast (50%) than at dinner (14%) lost more weight (5.1 kg difference) and reported better satiety than the other group following opposite meal patterns.
In conclusion, current evidence supports the fact that erratic sleep and eating patterns can cause circadian misalignments and cause a change in energy expenditure due to changes in physical activity, hunger levels and insulin resistance. This can negatively affect weight loss targets during an energy deficit.
18. Hydration
A study from the National Health and Nutrition Examination Survey (NHANES) reported a significant association between elevated body mass index and inadequate hydration.
While increased water intake benefits groups aiming to lose weight by improving satiety and reducing energy intake, dehydration itself is not directly linked to weight loss hindrance in research on humans.
Choosing water over calorie-rich drinks can reduce overall energy intake (up to 200 kcal), contributing to weight loss efforts.
19. Alcohol
Alcohol’s contribution to energy balance, beyond its caloric content, involves inhibiting lipolysis (fat breakdown), lipid oxidation and encouraging de-novo lipogenesis [132].
Excessive alcohol consumption can lead to impulsive behaviour, unplanned eating events and reduced energy debt [133].
Long-term alcohol consumption, even at low to moderate doses, is associated with insomnia [134], reducing energy expenditure due to sleep deprivation.
While studies report minor differences in weight loss related to alcohol consumption, probably from compensatory behaviour, the combined effects of inadvertent eating, sleep disruption and reduced fat oxidation hinder long-term weight loss progress.
20. Psychological factors
Certain psychological conditions, like Binge Eating (BE), are strongly linked to overweight and obesity, but when it comes to weight loss, the results are mixed. Ongoing BE, more than pre-existing BE, impedes weight loss efforts over 4 years.
Additionally, psychological factors, such as lack of willpower, self-sabotage, self-perception of body image and past stigmatizing experiences related to excess weight, emerge as barriers to weight loss and its maintenance in the long term.
Clinical depression and other emotional challenges may also lead to sedentary behaviour, overeating and difficulty in adherence to weight loss interventions.
21. Ultra processed foods
A study comparing ultra-processed and unprocessed diets [147] found that ultra-processed diets increased energy intake (~ 500 kcal/day) and correlated strongly with weight changes [148].
The inclusion of ultra-processed foods can drastically impact weight loss outcomes, particularly regarding sugar and fibre content.
There is a strong relationship between excessive sugar intake and weight gain [151].
This can likely be due to the response from the reward system that our bodies have developed to foods such as sugars [152] due to lesser satiety of sugary drinks [153] or both.
Fibre on the other hand improves satiety along with delay stomach emptying so you feel fuller for longer [154].
Different types of fibres have different physical structures, hydration properties, fermentability and viscosity [156] and have different satiety properties.
Recent studies [157, 158] have shown that some dietary fibre types might be better than others at inducing satiety.
Environmental factors
The external environmental factors of not losing weight reviewed include:
- Stress
- Social Support
- Weather
- Pollutants
- Plastics
22. Stress
Studies report an association between psychological stress (job-related or otherwise) and poor emotional health to weight gain.
However, stress does not always lead to weight gain in all groups. This can be because there is a difference in individual responses to stress.
When stress is reciprocated by comfort eating and sleep deprivation, such behaviours can contribute to increased energy intake.
Additionally, stress can hamper weight loss efforts, and can increase the probability of individuals dropping out.
A trial comparing groups receiving standard dietary and physical activity instructions that either followed stress management programs or had no such intervention. Stress management program participants lost more weight compared to the control group (1.36 kg/m2 difference in body mass index) [168].
Abdominal Fat
Stress is also linked to abdominal fat in particular. A previous study found that people with high cortisol (high stress levels in the body) have belly fat with 4x the number of cortisol receptors as anywhere else in the body.
23. Social Support
Many individuals do not know the role of social support in losing weight. Studies report that in-person or internet-based community support can aid in weight loss.
In a weight loss intervention study, a greater number of participants who were recruited along with friends completed the treatment compared to those who participated alone. The prior group even showed better weight loss maintenance.
In a survey including the internet weight loss community, themes such as encouragement and motivation, sharing of experience and information, recognition of success and friendly competition were valued and reported to be beneficial by the members.
24. Weather
Several studies show extreme temperatures and rainfall may lead to a reduction in physical activity and slower weight loss.
25. Pollutants
Short or long-term exposure to air pollution leads to increased cardiovascular risk [175].
This association is more prominent in old age, obesity and chronic disorders [176, 177].
There is some evidence to suggest a negative association between air pollution and intentional weight loss [178] and weight loss after bariatric surgery [179]. However, more studies are needed to investigate the extent of the effect on energy balance and weight.
26. Plastics
Plastic additives such as bisphenol-A (BPA) and nonylphenol are associated with body weight imbalance.
An in vitro study [181] has shown that these molecules encourage lipid (fat) accumulation. A further cross-sectional study also reported a positive association between BPA and diabetes.
Recent reviews summarized that several chemicals (obesogens), including those in plastics, can interfere with weight in multiple ways including promoting adipocyte number and size, interfering with hunger and satiety hormones, triggering insulin resistance and decreasing the resting metabolic rate.
CONCLUSION
So whilst this list is by no means exhaustive it does cover a lot of ground. And the good news is, there are a lot of factors within our control that can help shape how we look and feel from the inside out.
References
Dabas, J., Shunmukha Priya, S., Alawani, A. et al. What could be the reasons for not losing weight even after following a weight loss program?. J Health Popul Nutr 43, 37 (2024). https://doi.org/10.1186/s41043-024-00516-4

Recent Comments